Many believe that health technology will usher in a new era of healthcare, improving billions of lives. However, I am not so convinced.
If the health tech industry continues to build products for a select few rather than for everyone, it will fail to deliver the expected revolutionary change and will worsen health outcomes for the most disadvantaged in society.
So far, people in health tech have shied away from confronting the harsh realities of health inequity plaguing our communities. Instead of building technologies to solve these issues, there's an automatic default to the status quo of intending to do something about it but not actually doing anything about it.
Maybe the size or the scale of the challenge is too much. Still, turning health equity into just another buzzword, we accept its meaning as something aspirational, something nice to have and nice to say, something over there in the distance.
The result is health tech products on the market today exclude, neglect, and seriously misunderstand the people who would most benefit from these solutions.
For instance, the hotly anticipated news that Apple has developed a proof-of-concept device for needle-free continuous blood glucose monitoring has taken our feeds by storm. Pundits have already started to claim this is the end of diabetes as we know it.
I'm a tad more skeptical.
Looking into how Apple intends to measure blood glucose, the monitor uses optical absorption spectroscopy, which shines a light through the skin and measures glucose in the interstitial fluid.
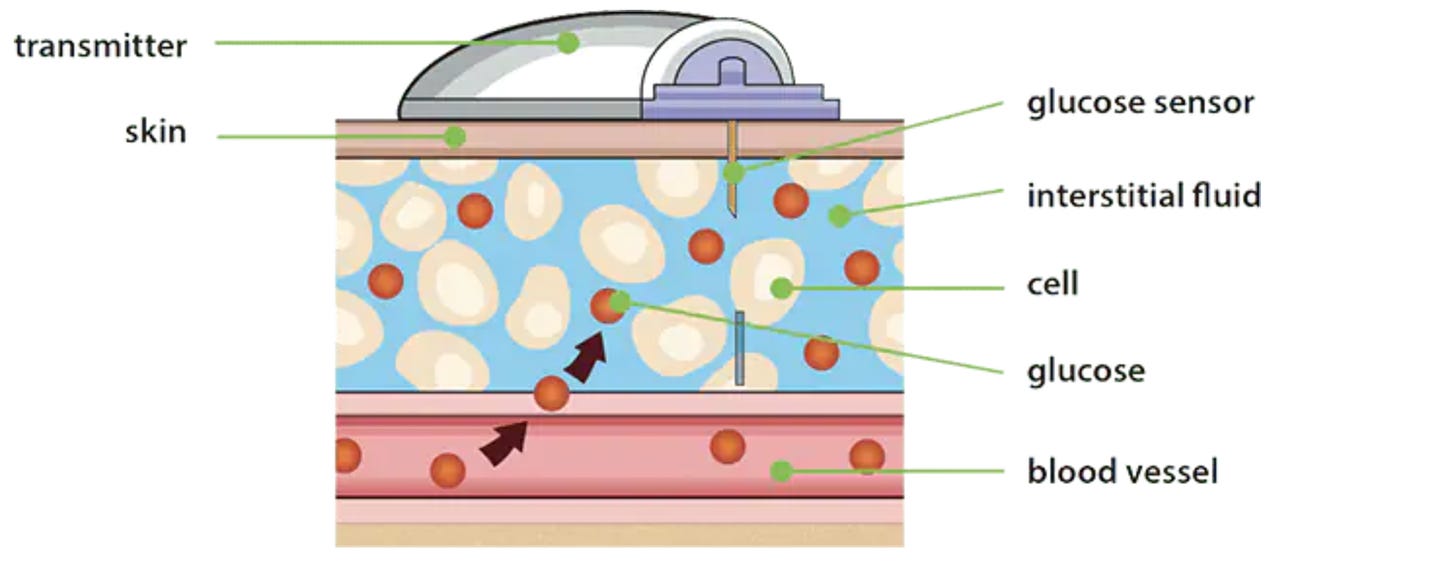
The problem is that wearable technology using spectroscopy has consistently shown higher error rates for people with darker skin tones and may not even work at all in some instances.
Professor Peter Colvonen from UC San Diego noticed the significant discrepancies in data when conducting a study on wearable technologies with white and black patients and was left scratching his head at the lack of diversity in validation studies.
Given that the chance of developing diabetes as a black adult is significantly higher than a white adult (66 more cases of diabetes per 1000 people), if Apple's CGM came onto the market today, it would simply be reinforcing the systemic inequity that exists amongst underserved communities.
The problem, then, is health technology causing an even more profound mistrust and skepticism from the very people we should be serving.
As Annie Jean Baptiste writes in her book, building for everyone, the moment we stop building with inclusivity in mind is the moment we start unintentionally excluding people.
And if you really peel back the layers of why we exclude people in health tech, ultimately, it boils down to the belief that underrepresented and marginalised communities do not have the power or income to make a product a success.
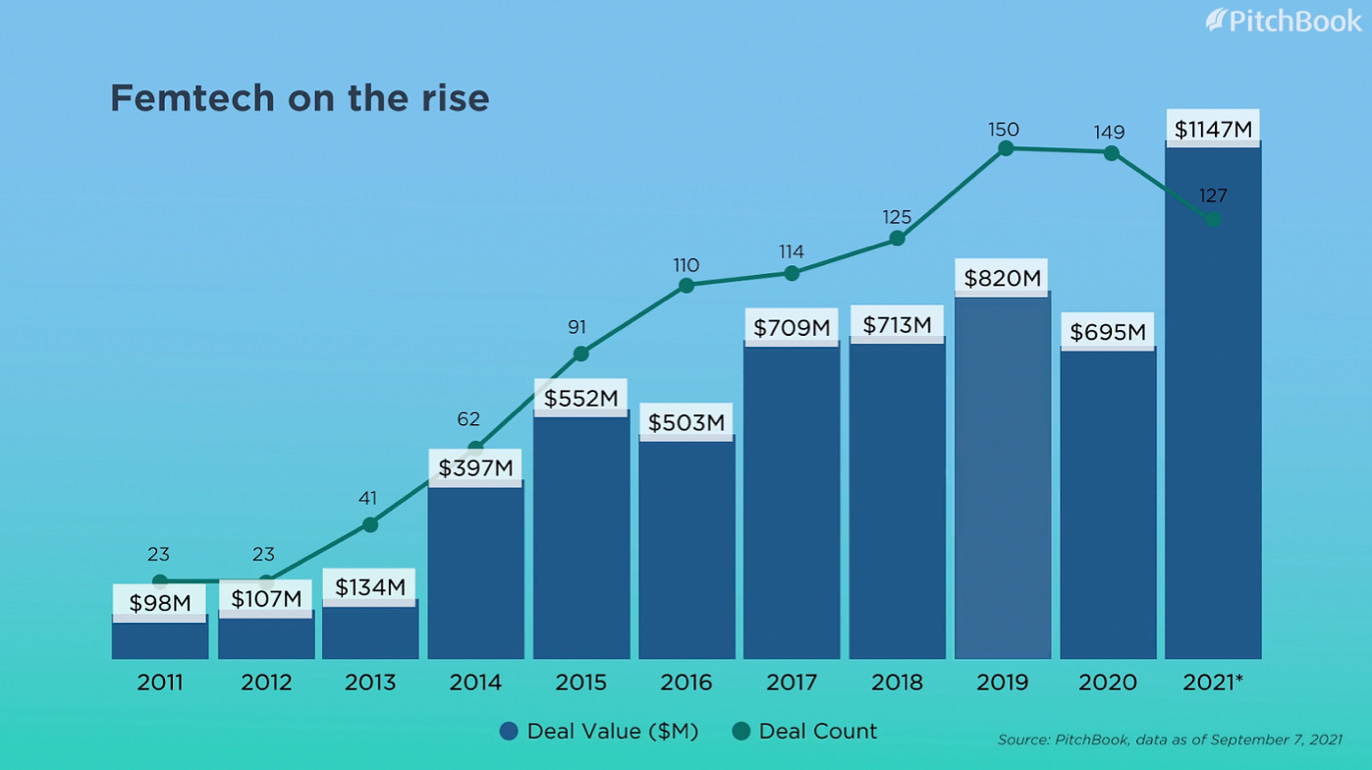
Just look at how long the industry ignored Femtech.
The lack of funding, stigma and underrepresentation of women in technology meant investors neglected the needs of over half of the world's population. Although the sector is finally undergoing its hockey stick moment, how long has it taken to get to this point and realize there are no groups of people we can exclude?
Unconscious bias or otherwise, believing people lack power or agency, is the cardinal sin that perpetuates and worsens health inequities.
Blinded by Ignorance?
Nearly 2 million people in the UK are living with significant sight loss, a number expected to double in the coming decades as people get older and live longer. They are often treated as existing on the periphery, and Telehealth solutions are not built for people with visual impairment in mind.
The lack of accessibility prevents patients from scheduling appointments online or navigating e-portals. It shouldn't come as a surprise then when nearly 60% of visually impaired people have stated difficulty accessing telehealth services.
However, I guarantee that if people with visual impairment were included in a telehealth solution's early product development stages, the result would be a better, more inclusive product for everyone.
There would even be the added benefit of tapping into new markets—an economic and societal success story.
Driving intention to action
Changing "well said" to "well done" will not happen overnight. For health equity to become a priority in technology, a strong business case must be presented with facts and figures about unexplored market potential.
It would be naive to think that impact alone will be enough to scale the product without considering the return on investment.
But health equity and profit do not need to be mutually exclusive, as Dr Jullian and Written Medicine in the UK have shown us. They have created business models that generate revenue and substantially impact underserved and marginalised communities.
Now what?
Once you've decided you want to make your health tech product more equitable, you can start casting your net wider and drawing your circle even bigger when you think about who could be impacted by the products you build.
Here are three crucial starting points to consider:
1: Designing your product: include a diverse population group, and try to understand how people from different backgrounds may perceive your solution. This is much easier if your product is in the ideation phase. So you have to plan early.
If you are further down the line in product development, you can still gain valuable feedback from a diverse user group and understand which potential markets you can explore.
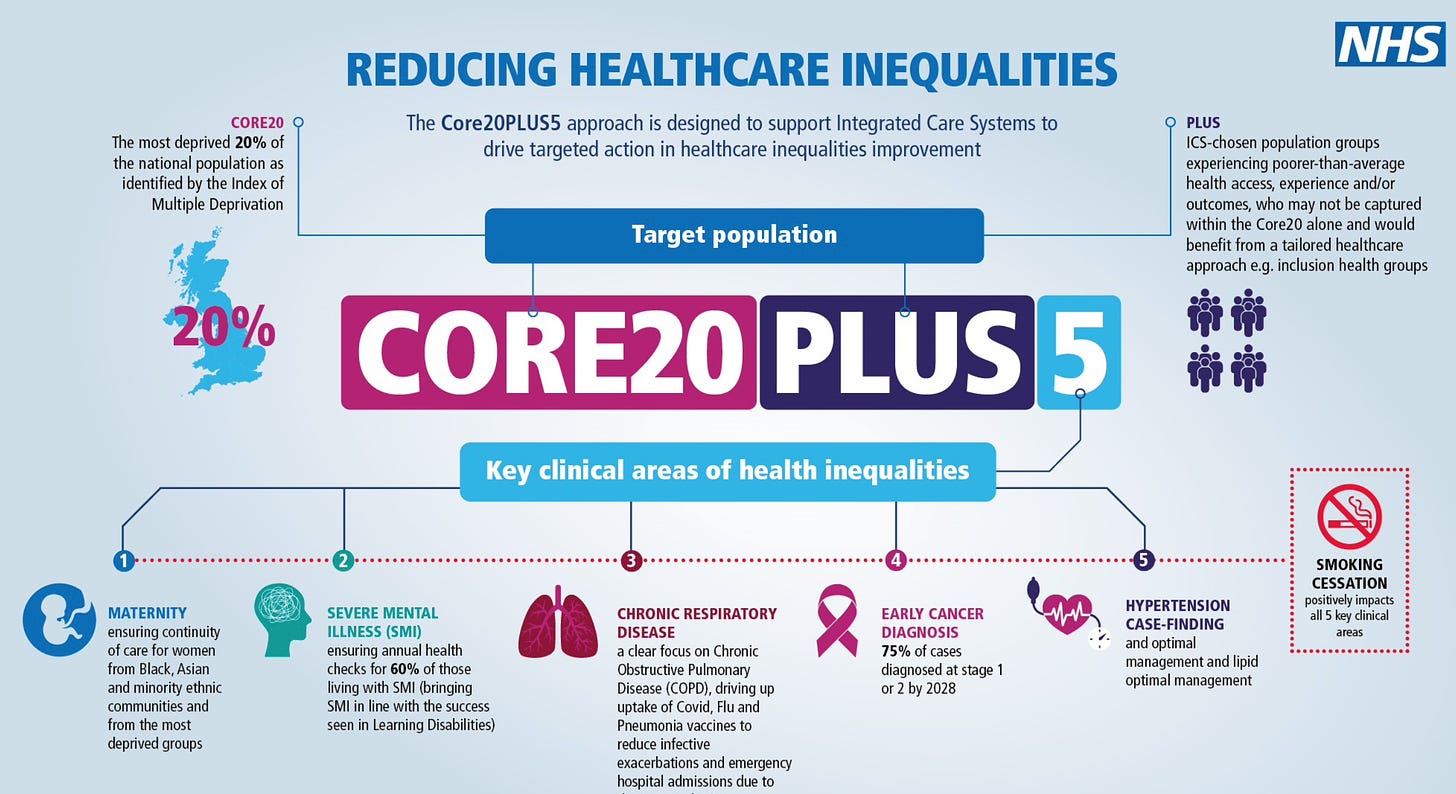
2: Who exactly do you target? This is a much harder question to answer and is the common stumbling block for many organizations. The simple answer is that if you are in the UK, the NHS has released its CORE20PLUS5, a national approach to addressing the inequalities faced by the most deprived 20% of the national population.
The initiative also includes five clinical areas that need rapid improvement, including serious mental illness and early cancer diagnosis.
3: Defining Objectives and Measuring KPIs: prioritizing health equity means you have to be clear what you are trying to accomplish, i.e making a product more appealing to users from a certain demographic.
You then need to measure performance (KPI) using agreed-upon metrics. If you treat health equity as a business function, you must know what you are measuring and what impact you are making.
This could mean collecting metrics on demographic data and understanding where your users are and how to meet a certain % of those in communities that are not engaging.
If you want to further your understanding in this area, I highly recommend reading Building For Everyone.
Final Thoughts
Addressing health inequity is hard. There are no quick fixes, but if we don't start doing this now, we will continue to build health tech products that worsen the divide between the haves and the have not's in society.
I don’t know. Being a typical millennial, I still see technology as a solution to most of the world’s ills. I just hope that faith isn’t misplaced.
This article was inspired by my time as a panellist at the NHS innovation accelerator interviews & from the works of Annie Jean-Baptiste & Prof Bola Owolabi (Core20Plus5)